Swiss researchers develop 3D-printed bioresorbable airway stents
Canadian Plastics
3D Printing Research & DevelopmentThe stents could simplify future treatments of upper airway obstructions.
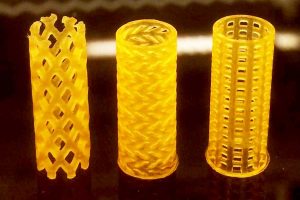
Three prototypes of the airway stents with different designs.
Photo Credit: Image from Paunovic N, et al. ScieAdv, 2020
It would hard to overstate the importance of airway stents in certain medical emergencies – if the trachea or the main bronchi narrows due to injury or illness, a patient gets too little oxygen, and risks suffocation. The tube-shaped stents inserted into the airway prevent that by bringing quick relief, but they’re not without disadvantages: Metal stents have to be removed surgically, which is a difficult process that’s often burdensome for the patients; and silicone stents often migrate away from the insertion site because the implants aren’t adapted to a patient’s unique anatomy.
But a research team from ETH Zurich university in Switzerland, working with researchers from the University Hospital Zurich and the University of Zurich, has now developed an airway stent that’s both tailored to patients and bioresorbable (gradually dissolving after implantation). These stents are manufactured using a 3D printing process known as digital light processing (DLP) and light-sensitive resins specially adapted for this purpose.
First, the researchers create a computer tomography image of a specific section of the airways. Based on this, they develop a digital 3D model of the stent. The data is then transferred on to the DLP printer, which produces the customized stent layer by layer.
In the DLP process, a building platform is immersed in a reservoir full of resin. The platform is then exposed to UV light at the desired locations according to the digital model. Where light hits the resin, it hardens; the platform is then lowered a little and the next layer is exposed to the light. The desired object is created layer by layer.
Until now, DLP technology could only produce stiff and brittle objects using biodegradable materials. To counter this, the ETH researchers developed a special resin that becomes elastic after light exposure – and the material properties of the object produced with it can be controlled by the length (molecular weight) of the macromonomers used and by their mixing ratio.
As soon as UV light hits the resin, the monomers link together and form a polymer network. Since the newly developed resin is too viscous at room temperature, the researchers had to process it at temperatures of 70 to 90°C.
The researchers produced several resins with different monomers and tested the prototypes they made from them to see whether the material is cell-compatible and biodegradable. They also tested the prototypes for elasticity and for mechanical stress such as compression and tension. Finally, the scientists used the material with the desired properties to make stents, which were tested on rabbits.
Inserting the stents also required a special instrument, as the 3D-printed objects must be delivered folded. The implants cannot be kinked or squeezed in the wrong direction and they must unfold perfectly at their site of deployment.
The researchers included gold in the stent’s structure in order to facilitate the use of medical imaging to track its location during insertion. This makes the stent more robust without changing its tolerability.
The tests on the rabbits conducted by the research group of Daniel Franzen, senior physician at the department of pneumology at the University Hospital Zurich, and the Vetsuisse faculty were successful. The researchers were able to show that the implants are biocompatible and that they are absorbed by the body after six to seven weeks. Ten weeks after implantation, the stent was no longer visible on X-ray images. In addition, the inserted stents generally did not move from their insertion site.
“This promising development opens up prospects for the rapid production of customized medical implants and devices that need to be very precise, elastic and degradable in the body,” said Jean-Christophe Leroux, professor of drug formulation and delivery at ETH Zurich. The process is still on a laboratory scale, and further research will focus on making the insertion of the stents as gentle as possible.
Source: ETH Zurich
